Hemorrhoids are commonly associated with rectal pain, itching, or bleeding. Back pain, on the other hand, is usually linked to muscles, discs, or posture. Because these two conditions seem unrelated, many people are surprised when they experience both at the same time. This leads to a reasonable question: can a hemorrhoid actually cause back pain, or is the overlap just a coincidence?
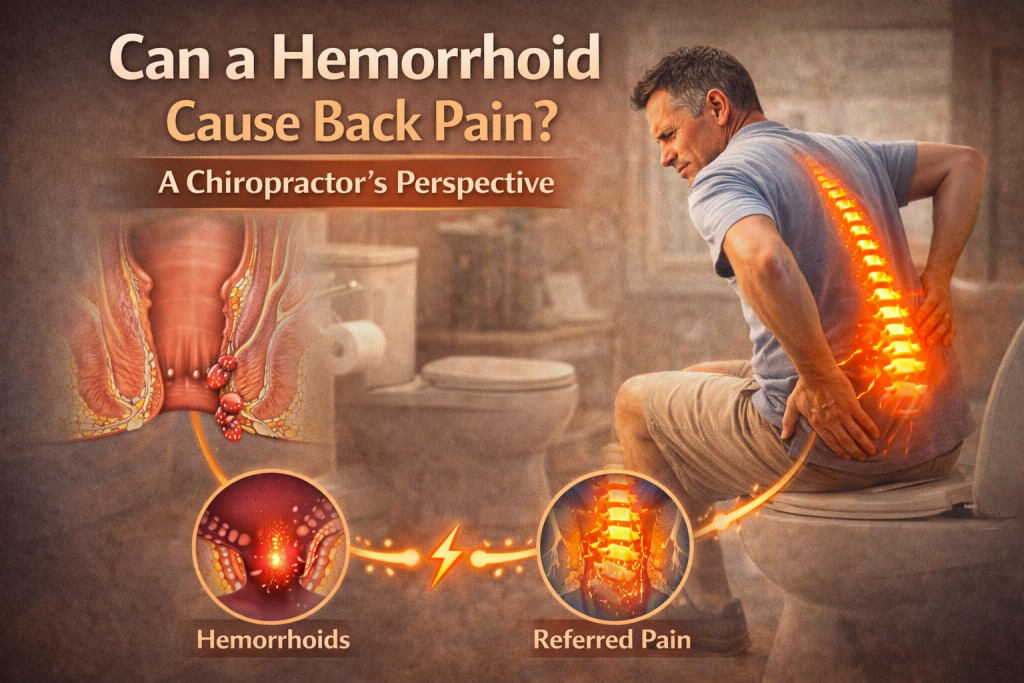
The answer is a definitive YES, but requires a closer look at anatomy, nerve pathways, and how pain can sometimes be felt far away from its original source.
Understanding What Hemorrhoids Are
Hemorrhoids are swollen veins located in the lower rectum or around the anus. They can be internal, forming inside the rectum, or external, developing under the skin around the anal opening. Hemorrhoids become a problem when increased pressure—often from straining, constipation, prolonged sitting, or pregnancy—causes these veins to enlarge and become inflamed.
Typical hemorrhoid symptoms include rectal discomfort, itching, pain during bowel movements, and bleeding. On their own, hemorrhoids do not involve the spine or back muscles. However, pain is not always experienced exactly where a problem originates.
Why Does Pain Not Always Felt at the Source?
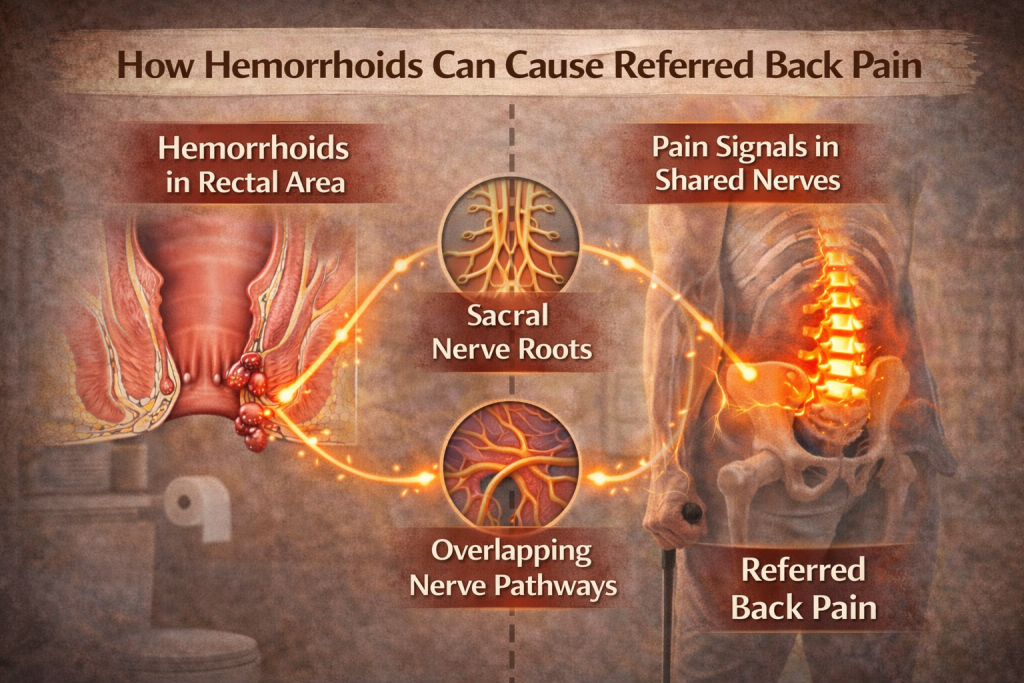
The body’s nervous system is complex, and pain signals do not always stay localized. This phenomenon is known as referred pain, where discomfort is experienced in a different area than its source. Pelvic organs, the rectum, and the lower spine share overlapping nerve pathways, through the sacral nerve roots.
Because of these shared nerve pathways, irritation or inflammation in the rectal area can be experienced as discomfort in nearby regions, including the lower back or sacral area. This does not mean the hemorrhoid is damaging the spine, but rather that the nervous system is sensing signals across shared pathways.
How Hemorrhoids May Indirectly Contribute to Back Pain?
In most cases, hemorrhoids do not directly cause back pain. However, they can contribute to back discomfort indirectly through several mechanisms.
Severe hemorrhoid pain can cause people to change how they sit, stand, or move. Avoiding pressure on the rectal area often leads to awkward postures, long time muscle tension, or uneven weight distribution. Over time, this disturbance can strain the lower back and surrounding muscles.
Chronic constipation, a major risk factor for hemorrhoids, also plays a role. Straining increases pressure in the belly and pelvic region, which can tighten core and pelvic floor muscles. Prolonged tension in these muscles may contribute to lower back discomfort, especially in individuals with a history of back pain.
When Back Pain Is Likely Not From a Hemorrhoid?
It’s important to be clear: back pain is rarely caused by hemorrhoids alone. If back pain is severe, constant, progressively getting worse, or experienced along with symptoms like fever, unexplained weight loss, numbness, or weakness, another cause should be considered. Seek medical attention if these symptoms persist.
Conditions such as spinal disc problems, kidney problems, infections, or gut disorders can cause both pelvic discomfort and back pain. In rare cases, serious rectal or pelvic conditions may present with referred pain to the back, but these situations typically involve additional warning signs beyond typical hemorrhoid symptoms.
Key Differences Between Hemorrhoid Pain and Spine-Related Back Pain
Understanding the nature of the pain can help distinguish whether hemorrhoids might be playing a role. Hemorrhoid-related discomfort is usually worse during sitting, bowel movements, or straining and may improve when lying down. Spine-related back pain often changes with movement, posture, or activity level and may radiate into the legs.
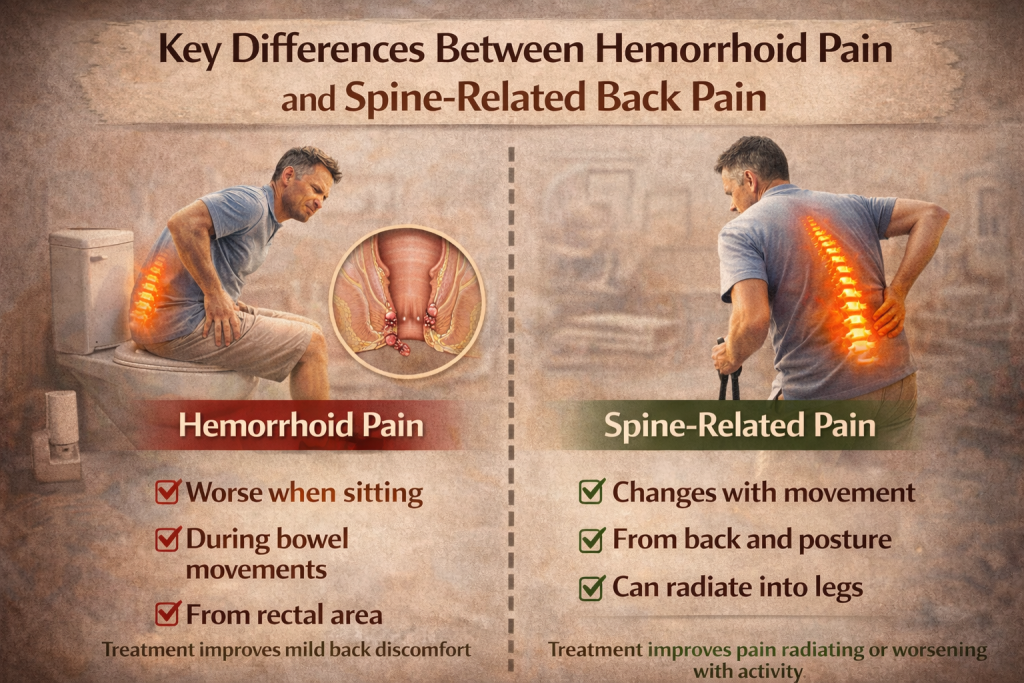
If treating hemorrhoid symptoms improves overall discomfort, including mild lower back pain, this suggests an indirect relationship rather than a primary spinal problem.
When to See a Chiropractor?
While hemorrhoids are common and often manageable at home, chiropractic evaluation is important when symptoms persist or overlap in confusing ways. A chiropractor can determine if the back pain is connected to a hemorrhoid problem, referred, or due to another underlying condition.
Seek medical attention if back pain is severe, progressive, or experienced along with weight loss and rectal bleeding that is heavy, persistent, or unexplained.
A Chiropractic Perspective on Pelvic and Back Pain
The body does not operate in isolation.. Pelvic health, bowel habits, posture, lifestyle habits, and spinal mechanics influence each other more than most people realize. Addressing constipation, reducing straining, improving sitting posture, and managing hemorrhoid symptoms can sometimes ease associated discomfort elsewhere in the body.
That said, hemorrhoids should not be assumed to be the cause of back pain without proper evaluation.
Conclusion: Can a Hemorrhoid Cause Back Pain?
Hemorrhoids do not typically cause back pain directly, but they can contribute indirectly through referred pain, altered posture, muscle tension, or associated conditions like chronic constipation. Mild lower back discomfort may occasionally accompany painful hemorrhoids, but persistent or severe back pain usually points to another cause.
The most accurate takeaway is this: hemorrhoids and back pain can be related, but they are rarely the same problem. Treating hemorrhoids may relieve discomfort, but ongoing back pain deserves its own evaluation.
